What is diabetic eye disease?
Diabetic eye disease refers to a group of eye problems that people with diabetes may face as a complication of this disease. All can cause vision loss. These diseases include:
- Diabetic retinopathy – This can be treated but not cured.
- Cataract – This can be treated and completely cured. Click here for more information.
- Glaucoma – This can be treated but not cured. Click here for more information.
What is diabetic retinopathy?
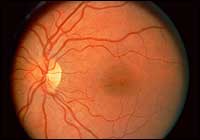
Appearance of a normal retina. The circular structure on the left side is the optic nerve. One inch to the right of the optic nerve is the “macula” which is where damage to one’s central vision occurs with diabetic retinopathy.
Diabetic retinopathy is a leading cause of blindness in American adults. It is caused by changes in the blood vessels of the retina. In some people, retinal blood vessels may begin to leak fluid leading to swelling of the retina (diabetic macular edema). In others, new blood vessels grow on the surface of the retina abnormally (proliferative diabetic retinopathy). These changes are vision threatening. Anyone with diabetes is at risk. The longer one has diabetes, the more likely he or she will develop retinopathy. Nearly 50% of all people with diabetes develop some degree of diabetic retinopathy during their lifetime.
Often, there are no symptoms in the early stages of the disease. Early detection is critical in attempts to treat this condition. As a result, every diabetic patient should have yearly examinations of the retina viewed through a dilated pupil. Vision may not change until the disease becomes severe. Blurred vision may occur when the macula (the central part of the retina) swells from the leaking fluid. This is called macular edema. If new vessels have grown on the surface of the retina, they can bleed into the eye, blocking vision. However, even in more advanced cases, the disease may progress a long time without symptoms. Regular eye exams are critical in the management of diabetic eye disease.
Treatment

Appearance of diabetic retinopathy. Notice the hemorrages in the retina which look like small red spots. Also, notice the small white flakes which are fatty deposits from leaking blood vessels. This leakage and fatty deposition is what causes visual loss.
Proliferative diabetic retinopathy can be treated with laser surgery which is done in the doctor’s office. A laser is a beam of light that is focused onto the retina. This light helps shrink the growth of abnormal or bleeding new blood vessels. Laser surgery has been shown to reduce the risk of severe vision loss for this type of retinopathy by 60%.
Diabetic macular edema is treated with laser as well. In this case, the laser light is used to seal off leaking blood vessels. However, laser surgery often cannot restore vision that has already been damaged. The main purpose of laser is not to improve vision but rather is an attempt to prevent progression of the disease. Here, again, is another reason that all diabetics must have yearly eye examinations viewed through a dilated pupil. Finding diabetic retinopathy early is the best way to prevent vision loss.
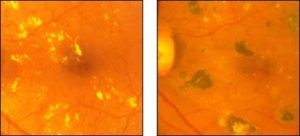
LEFT: The central part of the retina (macula) with fatty deposits before laser treatment. RIGHT: Significant reduction in fatty deposits threatening vision after laser treatment. The black spots are laser scars. Can diabetic retinopathy be prevented?
Diabetic retinopathy cannot be prevented. However, your risk can be greatly reduced. The Diabetes Control and Complication Trial (DCCT) showed that better control of blood sugar levels slows the onset and progression of retinopathy and lessens the need for laser surgery for severe retinopathy. The study found that the group that tried to keep their blood sugar levels as close to normal as possible had much less eye, kidney, and nerve disease. This level of blood surgar control may not be best for everyone, including some elderly patients, children under 13, or people with heart disease. Your internist or family physician should be consulted about which program is right for you. A woman who becomes pregnant and has previous diabetic retinopathy can have the retionopathy worsen during pregnancy. These patients need careful examination of the retina during this time period.
More information
To learn more about diabetic eye disease, write to:
National Eye Health Education Program
2020 Vision Place
Bethesda, MD. 20892-3655
See also: American Diabetes Association Web Site